Challenging Assumptions on the Economic Costs of Dementia
Health Economists GBHI Faculty Dominic Trépel and Atlantic Fellow for Equity in Brain Health Sanjib Saha share findings from recent research examining the health care costs of dementia.

Health care costs of dementia before, during and after diagnosis
Increasingly severe cognitive, behavioural, or motor symptoms due to the dysfunction and death of the brain’s nerve cells are the hallmarks of the diseases that cause dementia. There is no cure and, therefore, patients with Alzheimer’s disease, vascular dementia, or other dementias have a growing need for care as the disease progresses. With populations around the world ageing, the number of people experiencing dementia is increasing and so the associated global costs following diagnosis is assumed to be tending towards $2 trillion, thus creating major societal challenges and economic pressure to provide high quality care.
In this respect, we undertook a new study in collaboration with the Health Economics Unit of Lund University in Sweden, which has revealed previously unknown aspects of how health care costs develop over the course of the disease. Curiously, health care costs were significantly higher as early as 10 years before dementia diagnosis. And, while care costs increased, and indeed doubled, at diagnosis, our new research challenges existing assumptions about the economic implications of dementia as a few years after diagnosis, we saw costs drop to the same, or even lower, levels than in those without dementia. This raises real equity concerns for people living with dementia. For example, do people with dementia receive the health care they need as things get more difficult, or have our systems developed a tendency to displace the burden of care on others?
Our register-based study, published in Alzheimer's & Dementia: The Journal of the Alzheimer's Association, examines the full population of people living with dementia in Region Skåne in southern Sweden. These 21,184 people were first identified as having a dementia diagnosis between 2010 and 2016. Our research insights were made possible as individuals registered in Sweden’s national dementia registry can be linked to routinely collected healthcare data such as from primary healthcare, inpatient, and outpatient care. These data enabled our research team to examine individuals living with dementia over a 17-year period, including the year of diagnosis, 10 years before, and 6 years after diagnosis.
Our results support the brain health hypothesis that policy should take a life-course view in reducing the risk of dementia and support the growing idea that policymakers should allocate resources to reduce dementia risk factors, in line with high-level recommendations from the Lancet Commission on Dementia Prevention, Intervention and Care.
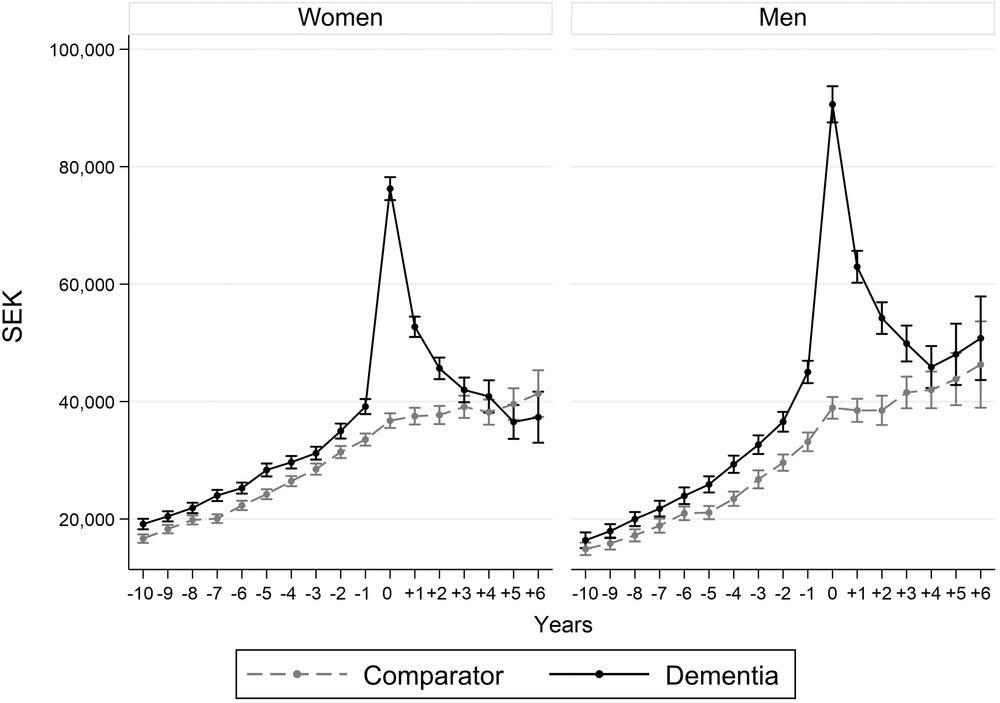
Figure 1: Predicted average health-care cost per patient at diagnosis as well as 10 years before and 6 years after by sex. 95% confidence intervals indicated by the whiskers. Expressed in Swedish krona, SEK, of 2016 prices.
What is driving dementia health care costs?
Our team is now undertaking further research, using state-of-the-art statistics methods, to explore what is driving the excess health care costs before diagnosis and why the marginal cost is lower in the subsequent years after diagnosis. For example, is the drop in health expenditure after diagnosis due to the initiation of treatments and social care provided by the municipalities, which substitutes for the need for health care? And if so, are costs being appropriately displaced onto social care, or onto families? And, could the initial increases in cost at diagnosis be related to difficulty in getting a definitive dementia diagnosis?
In conclusion, our findings suggest that people living with dementia have significantly higher costs compared to their counterparts long before the official diagnosis of dementia. To improve quality of life and to reduce the associated economic burden experienced by people living with dementia and their carers, this work mandates that future policies on brain health must: (1) be fit for purpose, and; (2) support timely identification of dementia, or indeed earlier changes in brain health.
The study was conducted at the Health Economics Unit, Department of Clinical Sciences, Malmö, Lund University, based on collaborative funding from Region Skåne and seven municipalities (Burlöv, Båstad, Lomma, Simrishamn, Vellinge, Eslöv and Örkelljunga municipalities), in collaboration with the Global Brain Health Institute (GBHI) and the Clinical Memory Research Unit at Lund University.
Contact
If you are interested in finding out more about this research please contact dominic.trepel@gbhi.org.
Publication: S. Persson, S. Saha, U.-G. Gerdtham, H. Toresson, D. Trépel and J. Jarl "Healthcare costs of dementia diseases before, during and after diagnosis: Longitudinal analysis of 17 years of Swedish register data." Alzheimer's & Dementia: the Journal of the Alzheimer's Association (2022) https://doi.org/10.1002/alz.12619
Authors

Sanjib Saha, PhD
Health Economist

Dominic Trépel, PhD
Associate Professor of Health Economics

